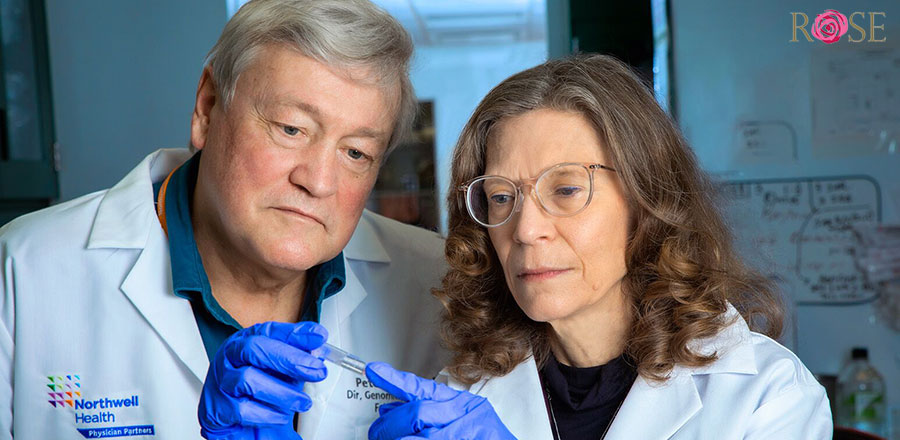
At EndoFound’s annual Blossom Ball on May 3, Christine Metz, PhD, and Peter Gregersen, MD, were honored with the 2nd Annual Women’s Reproductive Health and Endometriosis Industry Award. The professors at the Feinstein Institutes’ Institute of Molecular Medicine are co-founders and co-directors of the Research OutSmarts Endometriosis (ROSE) study, which EndoFound has supported over the past 10 years. The study, being conducted by a team of a dozen researchers, has six goals:
- Reduce the time between symptoms of endometriosis and diagnosis.
- Develop noninvasive (nonsurgical) methods to diagnose endometriosis.
- Discover improved treatments for patients with endometriosis.
- Better understand the cause(s) of endometriosis.
- Prevent progression of disease and alleviate the pain and suffering among patients with endometriosis.
- Learn more about uterine health and how endometriosis affects fertility.
EndoFound recently spoke with Dr. Metz about the history of the ROSE study, its progress toward its goals, and its future direction.
When did the ROSE study begin?
Metz: We started studying menstrual effluent (a complex mixture of blood, vaginal secretions, and endometrial [uterine] cells and tissues) about a decade ago. It had never been comprehensively studied in the context of human disease before, and it had never been seriously considered as a biological specimen to better understand the uterus, endometrium (inner lining of the uterus), or anything about women’s health. EndoFound gave us our first grant when we started the original ROSE study; without that, we might never have gotten it off the ground. Endometriosis is a small field in the scope of people’s health, and few back then believed we would be successful with the ROSE study.
You mentioned the original ROSE study, which you now call ROSE or ROSE I, and now you’re onto ROSE II. Explain ROSE I.
Metz: The purpose of ROSE or ROSE I was to distinguish menstrual effluent collected from healthy controls versus people who are already diagnosed with endometriosis. Over the past 10 years, ROSE has enrolled more than 3,000 participants from all over North America—most have provided samples and/or health and medical information. Participants fit into one of three categories: those with no symptoms of endometriosis, PCOS, or adenomyosis) [healthy controls], those who have undergone diagnostic surgery and have a confirmed diagnosis of endometriosis, and those who are symptomatic and have not yet undergone diagnostic surgery.
ROSE I is still going. We’re always enrolling subjects because we specific ongoing studies that are focused on investigating the cause(s) of endometriosis and exploring possible treatments. We isolate cells and freeze components of their menstrual blood for these studies.
And ROSE II?
ROSE II started over a year ago. In ROSE II, we are applying what we learned in ROSE I to menstrual samples from people who are symptomatic and are about to be diagnosed. So, we do it in steps. We’ve clearly seen differences between people who are already diagnosed with endometriosis and healthy controls, but that does not help diagnose people who are symptomatic because perhaps their disease won’t be as progressed.
How does ROSE II work?
We have about 100 patients enrolled and hope to reach 120 this summer so we can analyze our data in the fall. We’re currently enrolling patients who are symptomatic but have never been diagnosed with endometriosis before and are currently seeing a laparoscopic surgeon for a diagnosis. Some of the symptomatic subjects from ROSE I join the ROSE II study. We ask them to collect their menstrual blood before their diagnostic surgery so that we can compare our results with what we call “the gold standard” [diagnosis through laparoscopic surgery].
Are there challenges with that?
Metz: As we have learned, the gold standard is not exactly gold. The results of laparoscopic surgery can be quite variable, especially when performed by physicians who are not routinely performing the surgery. This has been a major stumbling block for us. Many patients have undergone surgery in which the surgeon takes only a couple of biopsies or doesn’t take any biopsies, and patients will not likely be diagnosed under these circumstances. We hear from many patients enrolled in ROSE I that they have undergone laparoscopic surgery two or more times before being diagnosed. Another challenge is that lesions can grow inward, making them difficult to visualize, and some lesions are just too small to visualize. However even with microscopic disease, patients can suffer with pain and other symptoms.
Along with the surgery being complex and sometimes uncertain, we have struggled to enroll in ROSE II because many patients are not referred for laparoscopic surgery, some prefer not to undergo surgery to be diagnosed, and there are issues related to the logistics of trying to collect a menstrual effluent sample prior to undergoing surgery. A woman could be signed up to have surgery in three weeks but won’t get her period in that timeframe. Also, they may be taking medications that suppress their periods. So, we’ve had challenges, and I think a lot of that will be improved with time and by targeting younger folks, including adolescents. Regardless, we must prove that we are able to detect changes in menstrual effluent in those patients who are diagnosed with endometriosis when compared to unaffected, healthy controls.
What is next for ROSE II?
Metz: After our analysis of our data from ROSE II in the fall, we hope to submit an application to the FDA to conduct a much larger multisite national study to prove that the markers we’ve identified do, in fact, predict endometriosis in patients who are symptomatic. We don’t know the number of patients we’d have to enroll in the multisite study. It will be driven by the results from the analysis of these specimens.
So, ultimately, your primary goal with ROSE is to have a noninvasive diagnostic test for endometriosis to shorten the time it takes for someone to be diagnosed?
Metz: We think of it as more of a non-invasive ‘screening test’ than a noninvasive diagnostic test. The hope is that someone would be incentivized by these markers that say it’s predictive you likely have endometriosis, and you really should undergo the diagnostic surgery to confirm it and to excise those lesions.
At the same time, we’re also investigating treatments. Currently, the only effective therapy for endometriosis is excision surgery. Pharmacologic treatments available today do not stop disease progression; they treat symptoms. So that’s another major effort of ours—to identify novel treatments that have not been envisioned. Most treatments are hormone-based. It seems that with many of women’s health problems, hormones are used as a treatment. However, most hormone treatments are accompanied by side effects—some of which can be miserable.
What happens after ROSE II?
Metz: We just keep going. Once we confirm or validate our screening method, we will have to test it in various populations. The one population we are most interested in is the younger set. This will require a separate study because we aren’t sure if menstrual effluent from a 16-year-old is equivalent to that of a 28-year-old. It’s just never been studied as a biological specimen, so very little is known.
Endometriosis has received significant attention in recent years. Along with the awareness and research, what more do you feel needs to be done?
Metz: I think one of the biggest problems we have is that many dabble in endometriosis surgery—doing one or two cases a month or less. We have no minimum standards for endometriosis surgery in this country. If you have had prostate cancer and are being monitored through prostate biopsies, there are minimum standards. For endometriosis surgery, we have zero standards. So there are many general gynecologists with limited expertise performing difficult diagnostic and/or excision surgeries, and while I think they mean well, additional education and training from the true experts in this field would improve their outcomes.
How hopeful are you about the recent attention women’s health in general has received?
Metz: It is so exciting! It’s almost becoming popular to be doing women’s health research. Dr. Jill Biden and President Biden just pledged $200 million for women’s health research. Also, I read that Melinda French Gates is starting her own philanthropic efforts with the $12.5 billion she received from the Gates Foundation upon her resignation. Her efforts will target women’s health and women’s rights globally. Now that it’s becoming more fashionable and there’s money for women’s health, you will see progress. A rising tide will lift all boats!